Romano A*, Parrinello NL, La Cava P, Tibullo D, Giallongo C, Parisi M, Vetro C, Conticello C and Di Raimondo F
Division of Hematology, University of Catania, Italy
* Corresponding author: Alessandra Romano, Division of Hematology, University of Catania, UOC Hematology with Bone Marrow Transplantation, Ferrarotto Hospital, Via Citelli 6, 95124 Catania, Italy
Received: March 16, 2016; Accepted: May 02, 2016; Published: May 04, 2016
ABSTRACT
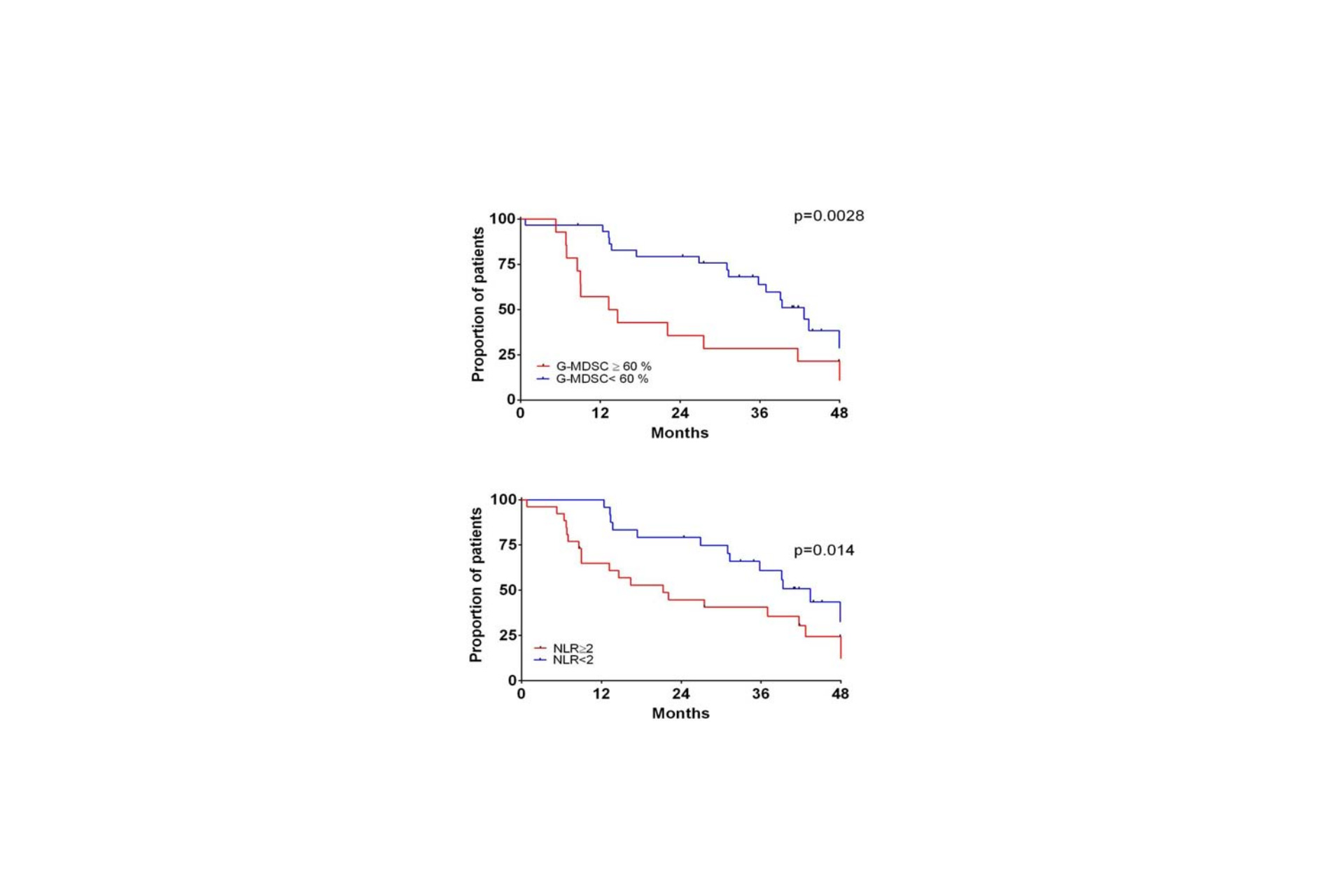
Background: Recent studies have indicated a role for the myeloid compartment in the biology of Multiple Myeloma (MM) and the neutrophil to lymphocyte ratio (NLR) is emerging predictors of progression free survival (PFS) and overall survival (OS) in MM. In addition, Myeloid-Derived Suppressor Cells (MDSC), a heterogeneous population of myeloid cells with peculiar immunosuppressive properties against T-cells, are increased in MM, as recently described.
Aim: We investigated MDSC and clinical variables at diagnosis (including NLR) and their impact on outcome of patients treated upfront with novel agents (Lenalidomide and bortezomib).
Methods: We evaluated by flow cytometry G-MDSC (CD11b+CD33+CD14-HLADR-) in 45 newly diagnosed MM patients treated upfront with lenalidomide (N=30) or bortezomib (N=15), compared to 50 MGUS and 30 healthy subjects matched for sex and age.
Results: G-MDSC percentage in MM whole blood was greater than healthy controls (61.2±1.6% versus 51.7±1.4%, p< 0.001) with a large overlapping with granulocytes. G-MDSC were higher in presence of extensive bone disease (p= 0.02), in patients carrying LDH ≥2 UPN (p= 0.0025) and fibrinogen ≥40 mg/dL (p= 0.01). G-MDSC were also positively correlated with neutrophil to lymphocyte ratio (NLR) recently described as a novel biomarker in MM (r2=0.60, p< 0.0001). G-MDSCwb was reduced after exposure to lenalidomide-based regimen (p< 0.0001) but not to bortezomib. Patients treated upfront with lenalidomide and G-MDSCwb >60% at diagnosis had shorter progression free survival (PFS) than those with less than 60% (16.8 versus 47.0 months, p= 0.04).
Conclusion: G-MDSC is increased in MM; they can predict response to lenalidomide. NLR could be surrogates for G-MDSC and this can explain the recently reported prognostic meaning.